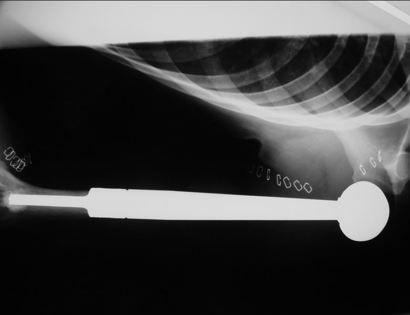
What is a Limb Sparing Surgery of the Entire Arm Bone?
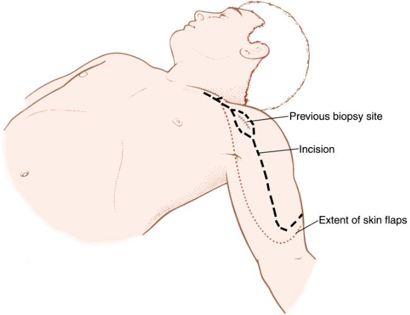
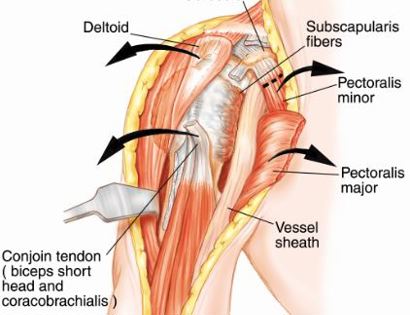
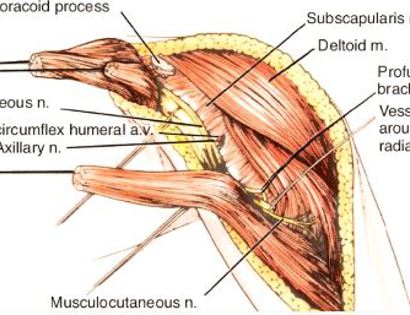
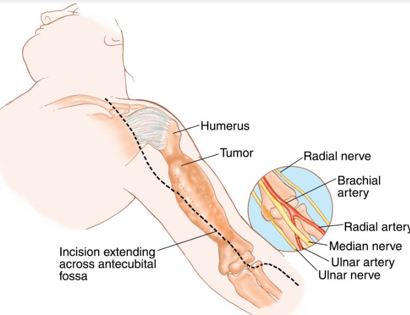
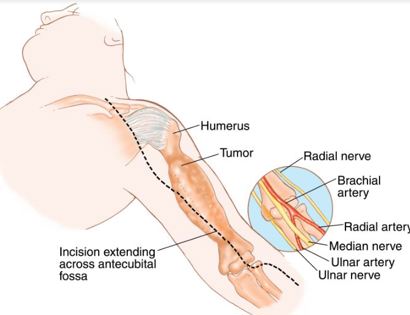
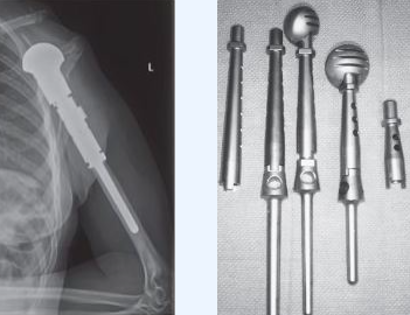
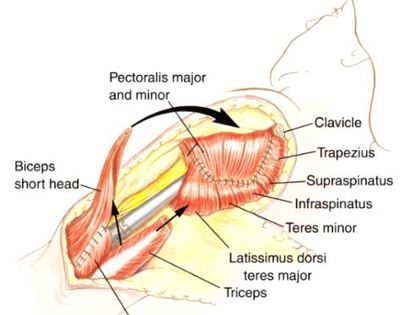
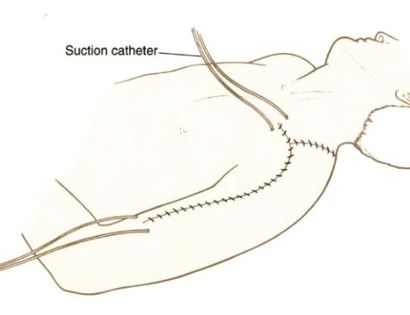
The entire arm bone, called the humerus, includes the shoulder and elbow joints. The shoulder girdle consists of the proximal humerus, scapula, and clavicle. The elbow consists of your humerus, ulna, and radius bone. Common tumors that affect the humerus are various sarcomas, benign aggressive tumors, and metastatic cancers to bone. Some of these tumors include osteosarcomas, chondrosarcomas, and giant cell tumors. Limb-sparing surgery can be performed for approximately 95% of tumors arising from this part of the body. In some instances, the extremity cannot be saved, and an amputation is performed. Contraindications for saving the limb may include neurovascular invasion, infection, pathological fracture, invasion of the chest wall, extensive disease, contamination from a poorly performed biopsy, recurrent disease.