Hemangiopericytoma
Hemangiopericytoma of the bone is a malignant tumor originating from the cells around tiny blood vessels called capillaries (called pericytes). It most commonly affects the pelvis, femur, spine, and humerus.
Hemangiopericytoma of the bone is a malignant tumor originating from the cells around tiny blood vessels called capillaries (called pericytes). It most commonly affects the pelvis, femur, spine, and humerus.


Hemangiopericytoma of the bone is a tumor or neoplasm that comes from the cells present at the walls of capillaries (tiny blood vessels).




Hemangiopericytomas are cancerous aggressive tumors that, if left unchecked, will grow and destroy your normal bone. Clinically, local pain and swelling may be the first signs. As the tumor slowly grows, the bone is weakened and you are at an increased risk of breaking the bone due to the tumor (called a pathological fracture). They may also spread to your lungs or other bones.
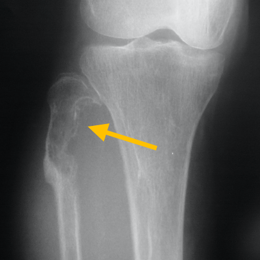
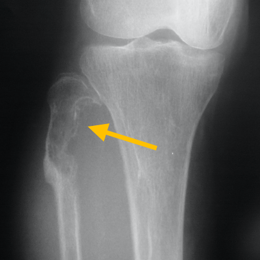
Radiographic imaging is used to help form a diagnosis. These include X-Ray, MRI, CT and Bone Scans.
An example of an MRI is shown.
Due to its rarity, there are no guidelines for its optimal treatment. Treatment should be aggressive and individualized. Treatment usually involves surgical removal and chemotherapy. Most patients are treated with a combination of surgery and chemotherapy. Most common treatment is wide radical limb sparing surgery. There are two kinds: round cell variation and hemangiopericytoma-like variation. Treatment for round cell variation includes a combination of chemotherapy, radiation and wide surgical resection. And for hemangiopericytoma-like variation includes chemotherapy and wide surgical resection only without radiation.
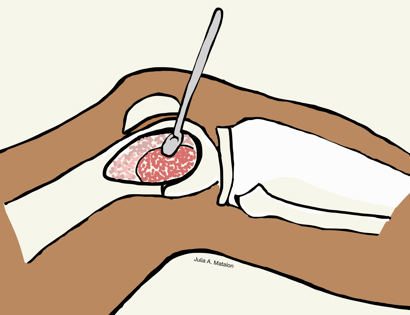
Intralesional Curettage means to scoop the tumor out using a spoon-like tool called a curette. This is a surgery that aims to remove the mass and restore the bone so that the patient can get back to normal function. The lesion is identified within the bone and scooped, or curetted, out. The cavity is then shaved down with a Midas Rex Drill, which is similar to a dental drill. This drill removes more tumor cells.
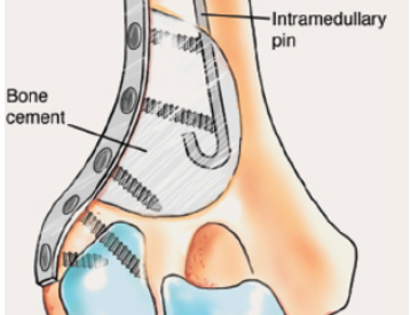
The empty bone cavity is usually filled with bone graft or bone cement. Bone can be donated (allograft) or taken from the patient themselves (autograft). Fixation devices, such as a plate and screws, may be used in specific situations to prevent postoperative fracture.

I've seen many doctors and I can confidently attest Dr. Wittig is the preeminent orthopaedic specialist. He is genuinely kind and caring, as he demonstrated by completely addressing my concerns and compassionately relating to what I was dealing with. He clearly outlined the plan of attack, and recommended the two additional doctors who would become part of my 'team'. Dr. Wittig was so effective in allaying our fears and bringing us optimism. My surgery was significant, but I was up and walking the next day and back at the gym 5 weeks later. This is further testament to Dr. Wittig's skill. He saved my leg and my life, and I feel so very blessed to say he is my doctor. I have already recommended him to others, and I will continue to do so. I would trust him with my closest family and lifelong friends. BEST DOCTOR EVER.
S.G.

Myself and my amazing team are dedicated to saving your life and your limb. Losing a limb because of a tumor can be a terrifying experience. But, it does not have to be the only option. I’ve spent 20+ years as a Board-Certified Orthopedic Surgeon and Orthopedic Oncologist.
I’ve devoted my career to helping children and adults afflicted with bone and soft tissue masses by performing complex limb saving surgeries. Most patients can have their limb saved, which may require innovative techniques.
Patients afflicted with musculoskeletal tumors have complex conditions that are best taken care of at large hospitals. I am the Chairman of Orthopedics and Chief of Orthopedic Oncology at Morristown Medical Center. My philosophy is a multidisciplinary team approach, working together to tailor treatment to individual patients. Education and research are essential to my practice, providing the best setting for extraordinary patient care. Because of this, we have some of the top results in the country.